Eye Surgery
Fuchs Dystrophy
Fuchs dystrophy is a common disease of the cornea. Fortunately, most people have such a mild case that it does not affect their vision and they may never be aware of the diagnosis. The disease affects a layer of cells on the back surface of the cornea that help to keep the cornea clear. If the cells are compromised, the cornea becomes more swollen and the vision becomes blurred.
Typically, people will experience worse vision in the morning. This is because the swelling of the cornea is less when the eyes are open and some of the fluid can evaporate into the air. When first getting up in the morning, the eyes have been closed all night without any evaporation taking place. Sometimes, aiming a hair drier at arms length at the eyes can help clear the vision.
Often people become aware of the condition when discussing cataract surgery with their eye surgeon. The reason is that cataract surgery can make the Fuchs dystrophy worse. In these cases, a person can come out of surgery with one problem gone (the cataract is removed) while the other condition is worse (Fuchs dystrophy). The result is that the vision may not be significantly improved and may even be worse.
The treatments for Fuchs dystrophy include using a salt-solution eye drops or a cornea transplant. The eye drops can sting but will help clear the vision by absorbing some of the fluid in the cornea. For more significant cases, the only solution is a cornea transplant. Fortunately, transplants have become much less invasive with better results.
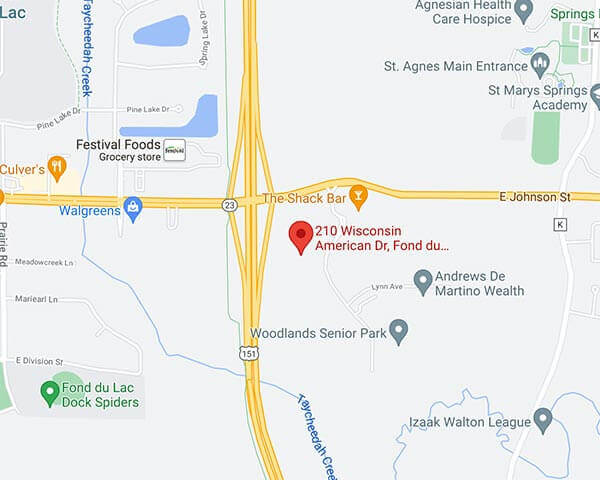
Dr. Larson and Dr. Raven are cornea specialists and takes care of many patients with Fuchs dystrophy. They regularly perform cornea transplants and are available for consultation at N.E.W. Vision Center.
No Drop Cataract Surgery
Why Everybody Loves It
We at Northeast Wisconsin Vision Center have been very excited about doing cataract surgery without drops. It is safe, effective and convenient for our patients.
How is it done? After the cataract surgery is complete, the surgeon irrigates the inside of the eye with an antibiotic. Then, a small amount of steroid is placed on the lower part of the outside of the eye (under the conjunctiva). A small white spot can be seen where the injection is made if the lower lid is pulled down. This spot will disappear over a few months.
Is it painful? No. This is done when the patient is under sedation and the eye is numbed.
Is it safe? Yes. Multiple studies have been done showing that doing an irrigation of antibiotic during cataract surgery decreases infection rates from 1/1000 using drops to 1/3000 to 1/6000 when using injections. These studies included thousands of patients – one included more than 20,000 patients.
Have others had surgery this way in Wisconsin? At Northeast Wisconsin Vision Center, we have done over 2,000 surgeries in this way with great success. We have had patients and referring optometrists very happy with the results.
Why do you like it? So many patients in the past had an easy time with the surgery but were frustrated using the drops. For some patients, family or friends were needed to help place the drops multiple times per day. This was inconvenient for all of those involved. The schedule was for 3 different bottles to be used four times a day (12 drops per day in the first week after surgery). In addition, many drops are very expensive whereas there is no extra charge to have the medications administered at the time of surgery.
Does anyone ever need drops? There are circumstances when drops may be used if other conditions exist. For some patients with diabetic retinopathy or glaucoma we may prescribe a drop. Also, there are rare occasions where drops are used to control eye pressure after the surgery. Most people using drops before surgery will need to continue them afterward.
Cataract Surgery
Drs Raven and Larson perform over one thousand cataract surgeries each year using the most modern techniques and equipment. The surgery has progressed to use smaller and smaller incisions with faster recovery and better results. Patients return home the same day of surgery with often little to no irritation and no sutures. While some sedation is used to keep patients comfortable, general anesthesia is not needed lessening the risks of surgery.
One of the most exciting advances are the lens implants now available for cataract surgery. Years ago, no implants were used and people needed thick “coke bottle glasses” after surgery to see properly. Today, not only do we not need thicker glasses, but often the glasses can be thinned and even eliminated. Near sightedness (myopia), far sightedness (hyperopia) and even astigmatism can be corrected by these lens implants.
The most advanced lenses are bifocal implants that help patients to see near and far without glasses after surgery. While traditional implants can help for one focal distance, these implants give focus to objects at distance and close. In this way, both eyes work together to see at all focal points similar to how a young child can focus without glasses. Some people in their 80s and 90s are able to see 20/20 at distance and read a newspaper – all without glasses.
The lenses may not be the right choice for people with other ocular diseases such as macular degeneration or advanced glaucoma. Drs. Merfeld and Larson want their patients to have the best outcome and will discuss all of your options with you concerning lens implant options.
Pterygium Surgery
A pterygium is scar tissue of the conjunctiva which can grow onto the cornea causing both irritation and decreased vision. It is most commonly from ultraviolet light and wind and is more common closer to the equator. Even in Wisconsin, however, people can be affected by pterygia and sometimes need to have them excised.
Dr. Larson and Dr. Raven are cornea specialists and they have special training in the removal of pterygia. The challenge of the surgery is that the pterygium is prone to come back since it is scar tissue. Several steps can be employed during the procedure to minimize the risk of recurrence. These include using an amniotic membrane transplant and mitomycin.
During the procedure, the eye is numbed to prevent any pain. The pterygium is removed and then tissue is placed where the pterygium was to prevent the recurrence.
If you have a pterygium and it is either large enough to cover the eye or causes frequent eye irritation, Dr. Larson would be happy to discuss you options.